ARTICLE OVERVIEW: Research into Spice and its ingredients is only beginning. However, we do know it’s a heavily addictive drug with both short and long term effects to your health. Withdrawal can also occur. This article gives you background into the physical and mental effects of Spice, and offers suggestions for where to seek help.
ESTIMATED READING TIME: 10 minutes.
Table of Contents:
- Spice Effects
- What Addiction Really Is
- Dependence vs. Addiction
- Denial
- Intervention Basics
- Help During Detox
- Help During Treatment
- How Many People Struggle
- Referrals to Help (Where to Find Help)
- How to Support a Friend
- Your Questions
Spice Effects
The herbal mixture “Spice” is a blend of both naturally dried plant material and synthetic sprayed cannabinoids. It’s advertised as a “healthy” marijuana substitute, which is anything but the truth. In fact, the chemicals found in Spice mixes have become a great concern in the medical field.
According to NIDA for Teens, people who have had bad reactions to Spice report symptoms like:
- fast heart rate
- feeling anxious or nervous
- feeling confused
- hallucinations
- increased blood pressure
- lowered blood flow to the heart
- paranoia
- suicidal thoughts
- throwing up
- violent behavior
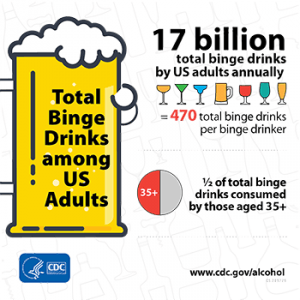
In a few cases, smoking Spice has caused heart attacks and death. You can find more facts about the effects of Spice on the National Institute on Drug Abuse NIDA website. The unpredictable dangers of Spice use have been outlined by NIDA here and in the following infographic.
What Addiction Really Is
According to the National Institute on Drug Abuse, addiction is a state when you no longer are taking a drug for the sake of feeling good. Rather, you’re taking it as a means of feeling normal. Further, addiction occurs when:
You continue to use a drug despite several negative consequences in your life.
But how does one make such a transition?
It begins the first time you take Spice. For a good amount of people, the high it gives you is a good feeling. Therefore, you want more of it. But, the more you take, the more your body adapts itself to the chemical compounds found within synthetic cannabis. This is known as a drug dependence. When you become dependent on Spice, you experience withdrawal when you lower doses or quit.
Over time, you need to smoke more Spice to get high. This is known as “tolerance”. When you’ve built a tolerance, you need more of Spice in order to feel its effects. This leads you to taking more and your body adapting further. Combined, this cycle eventually leads to compulsive behavior. It looks like this:
- Smoke Spice.
- Feel good.
- Repeat.
Dependence vs. Addiction
There’s a keen difference between addiction and dependence which should be understood.
An addiction is when drug use becomes compulsive even when it’s brought upon harmful consequences. People who are addicted to Spice have the inability to stop using it, despite negative effects to health, home, work, or school obligations.
Drug dependence can reinforce addiction. This is when the body adapts to the drug because chemicals are often present in the system. If Spice were suddenly taken away, withdrawal occurs.
So, how can you tell whether you dependent or addicted to Spice?
Signs and symptoms of addiction aren’t always visible or immediately obvious. There are a few questions you can ask yourself in order to find out.
- Have you ever tried to quit Spice without having success?
- Do you find yourself craving to use Spice?
- Are your responsibilities at risk due to your Spice use?
- Have you continued to use Spice despite it causing problems in your relationships (i.e. significant other, family, friends)?
- Do you find yourself in risky behavior due to the fact that you use Spice?
- Has your use of Spice affected previous activities you used to enjoy?
- Do you spend a large amount of time thinking about, obtaining, or using Spice?
If you’ve answered yes to one or more of the above questions, we suggest that you seek a professional diagnosis. It’s possible that you’re facing an addiction. And professional intervention can help!
Denial
Denial is a defense mechanism. People struggling with Spice often deny that they have a problem as a way of rationalizing their use and to avoid change. Denial is actually an inability to look at what’s really going on…seeing yourself as a “failure” is a difficult step to take.
So, how can you help a loved one break through denial?
First, understand a little bit more about where denial comes from. It’s common for people facing addiction to feel a deep shame of themselves. Both young people and adults don’t like to admit they’ve failed at self-control. Furthermore, many of us who deal with a drug problem want a good life…and have a difficult time when we don’t achieve it. This is why humans often use denial as a means of justifying behaviors.
When you’re in the early steps of helping anyone addicted to Spice, the first thing you’ll want to do is show support. Though it may not break through denial, it’ll lay the foundation of you showing care and acceptance for the person you care about. Here is a list of tips when it comes to helping someone look at denial:
- Attempt not to approach when they’re high on Spice.
- Be specific about what you talk about – bring up specific incidents which they’re aware of as a means of triggering memory.
- Discuss areas in which their drug use is having negative effects on other loved ones and, more specifically, their aspirations (careers, commitments, etc.)
- Keep in touch regular on the issues and any new issues to arise.
Additionally, there’s a chance mental health concerns are concurrent with denial, including depression and anxiety. This is especially true for Spice addicts, as synthetic cannabinoids have plenty of psychoactive properties which disturb thought and emotion. Therefore, when you look to address denial, you need to be very careful. Depending on the individual, you might be walking on thin ice and any wrong move can send the addict further into a drug hole.
It shouldn’t come as a surprise if your loved one continues to deny their addiction. This is common when it comes to compulsive drug use. It’s important to have a level of patience when dealing with these matters. And sometimes, in order to really break denial, you must go to further lengths.
Intervention Basics
Addicts generally don’t reach out until they’ve hit a point of despair through an incident or accident related to their addiction. As a family member, you want to do all you can as a means of avoiding this. The most efficient way to do so is through an intervention.
An intervention is considered to be one of the following:
1. A clinical or professionally arranged sit down discussion.
2. A close friend opening up for the first time about previously undiscussed behavior.
3. Work colleagues sitting together to talk for the first time about their concerns.
There is a risk involved in confronting an addict through such means. If you poorly plan or manage the intervention, it can result in:
- Bitterness
- Hostility
- Resentment
- Violence
With that in mind, here are some suggestions for early and effective intervention. If you’re looking for a professional interventionist, you can search the Association for Intervention Specialists, AIS Directory. Here are some basic guidelines.
1. Carefully Choose Who Will Attend. Spice has many psychological and emotional side effects. Therefore, you’ll want to be keen on who is present during the intervention period. You want to create the right dynamic. Not everyone is capable of this.
2. Get Some Advice Before You Begin. Go to an addiction counselor or professional who has experience in conducting interventions before you attempt to talk about the problem with your loved one. These professionals can inform you of the important points to cover and how to go about conversation throughout the intervention.
3. Plan Communication in Advance. Accusations don’t work. Rather, you want to help a loved one understand their problem and give them aid in recovery. Therefore, the way you communicate is vital. Some people have difficulty with this as they might’ve been harmed through the individual’s addiction. It’s important to keep specific in why you’re holding the intervention, emphasize on your love and support, and don’t exaggerate your emotions.
4. Be Prepared for Anything. There’s no telling how a person will react to an intervention. Some individuals will understand while others will retaliate. Consider the mindset of the person struggling with addiction and the time in which you choose to conduct the intervention. You should prepare yourself as much as possible for any reaction they may give and develop a comprehension of how to handle it properly.
5. Follow Through. The intervention is only the first step towards recovery. Make you follow through, go through intake with a rehab clinic, and become a part of the recovery process. Family counseling can be incredible helpful and can change your family dynamic for the better!
Help During Detox
Luckily, when it comes to Spice, detoxing generally isn’t as painful as it is when it comes to other drugs, such as opioids or alcohol. This is because there’s less of a physical dependence in comparison to a psychological one.
Still, Spice withdrawal can present a similar pattern. Common physical symptoms brought upon by Spice detox include:
- Agitation and irritability
- Cravings
- Depression
- Extreme sweating
- Headache
- Insomnia
- Loss of appetite
- Mood swings
- Uncontrollable vomiting, nausea, and diarrhea
Although withdrawal from Spice has not been fully defined, some symptom relief has been reported with benzodiazepines and the atypical antipsychotic, quetiapin. Further, when looking to help someone who’s going through the detox process, you’ll want to be keen on the danger of dehydration. Make sure the person recovering gets plenty of water taken in small amounts. This will ensure the body to stabilize back to its normal chemical functioning.
However, a bigger concern loved ones will have when handling Spice withdrawals is that of mental health. Since Spice is primarily a psychological substance, the biggest issues with it pertain to that of the mind. Though these are apparent throughout detox, they truly peak during treatment.
Help During Treatment
Addiction treatment is most effective when it’s a combination of medications and talk therapy. In fact, a variety of psychotherapy options are available. The purpose of talk therapy is to help former drug users to adjust back to day-to-day functions without the need for their drug-of-choice. This is done through teaching people how to handle emotions and behaviors while attempting to reduce cravings. On top of this, medications help people stable mood. This is why antidepressants may be prescribed in the first 3-6 months of treatment.
Psychotherapies generally last anywhere from three to six months and sometimes upwards to a year, depending on the level of addiction. There are a variety of things you can do in order to ensure your loved one gets the best out of treatment.
Be Present at Family Therapy Sessions. People facing addiction usually go through group therapy and individual counseling on their own in rehab. However, when it comes to the participation of loved one, family therapy is the most efficient. The goal of these therapies is to figure out the underlying cause of the drug addiction while working towards rebuilding relationships. This is also a good moment to work out any personal complications that may have arose during your loved one’s addiction.
Promote General Good Healt. Besides therapies and medications, many family and friends look into healthy living as a means of helping their loved one. These can be anything from exercise and yoga to meditation and creating art. By influencing these hobbies, you’re showing your support through a new means.
Always Be There. Treatment is difficult and, more often than not, people going through it will feel guilt, shame, and remorse. Not only must they push through all sorts of therapies but they must also keep down the itch of cravings and focus on a new life ahead. As a person of support, it’s vital you’re always there for them. Showing this can make a huge difference and motivate your loved one.
The Number of Current Users
One thing that can give you some sense of relief is that you are not alone. While synthetic marijuana is still very new, statistics about how many people are currently affected by Spice are tracked by government and health agencies.
- In 2010, 11,406 people were rushed to the ER due to associations with Spice. 77.5% of them were male and 22.5% were female. 75% were between the ages of 12 and 29.
- In 2016, the Monitoring the Future Study found that 3.7% of high school seniors had taken Spice at least once in the prior year.
From these statistics, NIDA found that Spice is the #2 most used drug after marijuana on the illicit market for young people. And of those using it, most are young males.
Where to Find Help
You have a variety of options at your disposal when looking for help for a loved one. These include:
- Addiction doctors (Find an ABAM specialist)
- Psychotherapists or counselors (Find an APA psychologist member near you)
- Psychiatrists (Find an ABA psychiatrist near you)
- Social Workers (Your state’s Department of Health and Social Services)
- Substance Abuse and Mental Health Services Association’s (SAMHSA) National Hotline 1-800-622-HELP (4357)
- You family physician
How to Support a Friend
If you’re a friend of someone who’s addicted to Spice, you might want to read through the information about for families. Know that it’s important you help them separate from the crowd of people who are using. And you can list facts to present to your friend about your concerns. Other than that, there’s really not too much that you can do.
Once out of treatment, relapse will remain a possibility. A high percentage of people relapse due to being in the wrong environment. In this way, the most important thing for you to do is offer any motivation towards a sober lifestyle. Support good habits and you’ll be super helpful to your friend!
Your Questions
We hope to have answered your main questions about helping someone seek help. But we know that you may still have something to ask.
If you have any further questions about how to help a Spice addict, we invite you to ask them in the comments below. If you have any advice to give for people currently trying to help a Spice addict, we’d also love to hear from you. We try to provide a personal response to each comment and get back to you promptly.