ARTICLE OVERVIEW: Opiate drugs are some of the most addictive out there and, likewise, some of the hardest to quit. Yet, with the right kind of help, it’s entirely possible. This article reviews how withdrawal is hard and the reason behind it, describes symptoms occurring along the basic timeline, and informs on directions for help.
ESTIMATED READING TIME: Less than 5 minutes.
Table of Contents:
- Is Opiate Withdrawal Hard?
- Opiates and the Brain
- Is Opiate Withdrawal Dangerous?
- A List of Withdrawal Symptoms
- Duration
- The Basic Timeline
- Medicines that Help
- Natural Remedies that Help
- Where to Go for Help
- Your Questions
Is Opiate Withdrawal Hard?
But why is opiate withdrawal so hard?
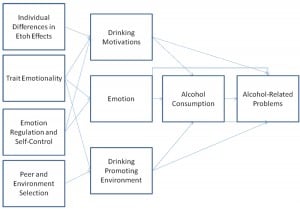
The main reason opiate withdrawal is so hard is because of the severely uncomfortable symptoms, such as restlessness, anxiety, headache, sweating…. If you’ve ever had a period of time without “your fix”, then you’ve most likely already experienced the initial stages of withdrawal. So, the answer has to do with the way the brain adapts to opiates over time.
Opiates and the Brain
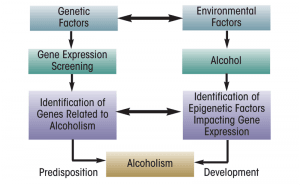
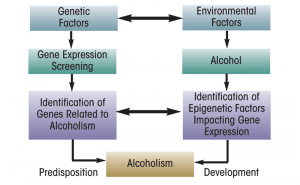
What happens in the brain, exactly?
When you take an opiate, the chemical enters the brain and attaches to a variety of opioid receptors. Particularly, those involved with pain and pleasure, such as the reward system. These receptors are located in different areas of the brain. From these opioid receptors, the opioid triggers neurotransmitters throughout other areas of the brain and body.
This transmission leads to euphoria. It also leads to pain relief. Due to an opiate’s chemical effects of the body, users may also feel the following:
- Dry mouth
- Flushing of the skin
- Heaviness
- Itching
- Nausea/Vomiting
When you stop taking an opiate – even just for a short period of time – withdrawal symptoms occur primarily due to your physical dependence. Once you’re drug dependent, the body and brain adapt to the drug as “normal”. The brain counterbalances the depressant effects of opiates by triggering stimulant chemicals and functions. But take away the drug, and your brain and body are left with the unnatural stimulant effects until they balance out again in detox. This usually takes between 7 to 10 days.
Is Opiate Withdrawal Dangerous?
Can you undertake detox and withdrawal from an opiate drug on your own?
You might assume so, but the problem with this assumption is that probably you’re NOT a medical professional. Treatment facilities have a way of treating withdrawal to:
1. Ease withdrawal symptoms.
2. Offer a medically supervised and controlled environment.
3. Give you an opportunity to process your thoughts and understand emotions.
Attempting to quit on your own terms IS dangerous because you have no idea how your body and brain react. And when symptoms become overwhelming, you won’t know what to do. Furthermore, without a supportive environment, relapse becomes more likely. Studies show that between 40% and 60% of people addicted to opioid drugs end up relapsing.
The safest way to withdraw from opiates is at a medical detox. Give yourself the gift of successful recovery and seek treatment.
A List of Withdrawal Symptoms
So, once you decide you want to quit, you need to prepare. Your body and brain will need time to readjust back to its native, original chemical balance, a state known as homeostasis. This time of adjustment is called withdrawal; withdrawal manifests as a specific set of symptoms.
Have you ever gone a day or two without getting your fix?
Have you noticed your body beginning to feel highly uncomfortable?
These were the early stages of withdrawal. These symptoms include:
- Agitation
- Anxiety
- Increased tearing
- Insomnia
- Muscle aches
- Runny nose
- Sweating
- Yawning
As opiate withdrawal progresses, the above symptoms become more intense and the following symptoms kick in:
- Abdominal cramping
- Diarrhea
- Dilated pupils
- Goosebumps
- Nausea
- Vomiting
Symptoms usually begin about 12 hours after your last exposure to an opiate drug.
DURATION
Detox generally lasts around 7 days and begins between 6 to 12 hours after your last dose. For the following 1 to 3 days, your withdrawal symptoms will peak. Then, over the course of 5 to 7 days, symptoms will gradually die down.
Still, there is no clear answer. The amount of time an opiate detox takes depends on:
- Your age.
- Your personal metabolism.
- Usage amount.
- Length of use.
For example, older individuals who’ve been using for a longer period of time are much more likely to experience more intense and longer withdrawals than those who’ve been using only a few weeks at smaller doses.
There are two different types of withdrawals that will persist during detox:
1. Acute Withdrawal – Begins with feelings of anxiety and cravings, climaxes around 36 to 72 hours, and decreases heavily within the following 5 days.
2. Protracted Withdrawal Symptoms (PAWS) – Will follow acute withdrawals and can last up to months.
The Basic Timeline
Day 1 to 2 – Usually the most difficult to get through, as the harshest withdrawal symptoms manifest during this time. You can expect to feel light symptoms of discomfort around 12 hours after your last use. The most notable symptoms you’ll experience are muscle aches and pains.
You will also have some combination of dilated pupils, sweats, chills, nasal stuffiness, watery eyes, irritability and possibly stomach cramps and diarrhea. Depending on how much your body depends on opiate drugs, you may experience extreme muscle pain during this time. Along with this, you’re also likely to feel the following symptoms:
- Anxiety or panic attacks
- Chills
- Diarrhea
- Loss of appetite
- Trouble sleeping
Day 3 to 4 – You can expect the worst of your discomfort to pass during this time, but it’s not entirely over. As the medical professionals supervising you will remind you, it’s important to stay hydrated. The most uncomfortable withdrawal symptoms to be expected are those you experience in the first days, plus:
- Abdominal cramps
- Increased blood pressure
- Increased heart and breathing rates
- Nausea
- Shivers
- Sweating
- Vomiting
Day 6 and Beyond. During this time, the withdrawal symptoms usually ease down. The body is getting back into homeostasis. There are some factors of withdrawal which may persist, such as trouble sleeping and/or eating as well as nausea and anxiety. However, for the most part, the body has finished detoxing and the mind is ready to undergo psychotherapies – a treatment which sets out to reduce cravings and change an individual’s conduct based around their prior drug use.
Since psychotherapies play a role in the withdrawal timeline, there’s no accurate way to tell how long you’ll have to undergo treatment. Generally speaking, most people who want to address an problems with opiate drugs do well with medical supervision for the following 3 to 6 months. Medication assisted treatment and talk therapy are key to a full recovery. However, some people remain in some form of a treatment program for months to years as they find a support system keeping them from relapse.
Medicines that Help
- Buprenorphine – A partial opioid agonist, which binds itself to opioid receptors, just not to the extent of a full opioid agonist. In turn, this reduces withdrawal symptoms and cravings, giving individuals a better chance to prevent relapse.
- Loxifidine – Approved by the Federal Drug Administration’s (FDA), loxifidine has been known to greatly reduce withdrawal symptoms. Though it can’t treat drug addiction in and of itself, it’s one of the most popular medications when treating opiate addiction.
- Methadone – Since the 1960’s, methadone has had great success in reducing withdrawal symptoms and, in some cases, even delaying them. Methadone attaches itself to opioid receptors, similarly to other opiate drugs. This effectively makes the user craves less and gives them a better chance to prevent relapse. It should be noted, most people are only on methadone for a short period, as it can be an addictive medication if misused.
- Naltrexone – A blocking action against opioids which isn’t addictive nor sedative. Taking this blocker medication is an option once you’ve gone through withdrawal and begin psychotherapy. It will make it impossible for you to fell euphoric if you do take opioids.
In order to better understand which medication(s) is right for you, you’ll want to consult your doctor.
Experts find that medication in combo with psychotherapy are the most beneficial form of treatment. The idea is that you stabilize your physical state and then address your mental state. Reducing compulsive urges helps you focus on deeper aspects of healing.
Natural Remedies that Help
However, you’ll want to address specific symptoms.
Since many withdrawal symptoms are similar to the flu, there are natural remedies out there to ease discomfort. For example, traditional herbal preparations of China and India have anti-addiction effects with less adverse effects than alpha2-adrenergic or opioid agonists. If we take a look at individual symptoms, we can figure out how to treat them.
Chills. A flu-like symptoms many people experience during detox are chills or cold-sweats. Constant shivering is usually a major factor of this. In order to warm yourself up, it’s suggested you wear extra layers such as sweatshirts or cardigans. Hot pads and warm, long showers or baths can also help. Kratom (Mitragynia speciosa korth) is recognized increasingly as a remedy for opioid withdrawal by individuals who self-treat chronic pain.
Nausea. Since symptoms of nausea have much to do with the food and liquids you intake, you can eat and drink certain things as a means of reducing the discomfort. These include, but aren’t limited to:
- Bland foods, such as bananas, rice, or toast.
- Eating several small portions of food throughout the day rather than a few large meals.
- Avoiding foods that are high in fat and grease.
- Taking small sips of water often. Dehydration is a huge concern when it comes to withdrawal and it’s vital you intake lots of water. Instead of drinking a large amount all at once, it’s suggested – for nausea’s sake – you take a little at a time.
Shaking. In a study done by Pharmaceutical Biology, rats were tested on to see if the herb Hypericum perforatum (or St. John’s wort) could reduce the shaking involved in opiate withdrawal. Not only did the shaking cease but researchers also found the rats’ diarrhea to reduce. Another way people reduce shaking is by quitting caffeine when they quit opiates. Caffeinated drinks are known to aggravate shaking and trembling tendencies.
Trouble Sleeping. Though it’ll be difficult to hop right back into a healthy sleep schedule, you want your body to have a clock of its own. This means you’ll want to develop a schedule for when you fall asleep and when you wake up. So, lying in bed at the same time every night helps. Furthermore, you might want to consider where you’re sleeping. Many people enter an inpatient program, where sleep environment cannot be controlled. Still, if you sleep better in a cooler or warmer temperature, this is something you can ask for.
Where to Go for Help
But where to look?
- Addiction doctors (Find an ABAM specialist)
- Detox clinics. Search the Substance Abuse and Mental Health Services Administration’s (SAMSHA) Treatment Locator or call their National Helpline – 1-800-622-HELP (4357)
- Psychotherapists or counselors (Find an APA psychologist member near you)
- Psychiatrists (Find an APA psychiatrist near you)
- Social workers (Your state’s Department of Health and Social Services)
- SAMSHA Opioid Treatment Program Directory
- Your family physician
You’ll also want talk to your family and friends. The reason for this is throughout your journey to recovery, they’re going to be your support system. The people you can always turn back to when things get too difficult. Furthermore, they can help guide you along the rest of the recovery process. If you’re a family member or friend of someone who’s addicted to crack there are a variety of options for you to seek help for your loved one.
And when you want to find the right treatment facility, give us a call. We’re happy to help.
Your Questions
Reference Sources:
NIDA: Understanding Drug Use and Addiction
NIDA: Heroin
NIDA: HEROIN: What Effects Does Heroin Have on the Body
NIDA: What are the Long-Term-Effects of Heroin Use?
NCBI: Clinical Guidelines for Withdrawal Management and Treatment of Drug Dependence in Closed Settings
NIDA: Drugs, Brains, and Behavior: The Science of Addiction
Medline Plus: Substance Use Disorder
Addiction Blog: What is rapid opiate detox? Does it work and is it safe?
U.S. Pharmacist: Acute Opioid Withdrawal: Identification and Treatment Strategies
SAMHSA: Protracted Withdrawal
NCBI: Opioid Dependence Treatment: Options in Pharmacotherapy
NIDA: Effective Treatments for Opioid Addiction
Medical News Today: Can You Treat Opiate Withdrawal Symptoms at Home?
Taylor Francis Online: Journal – Pharmaceutical Biology: Nature Cures Nature: Hypericum perforatum Attenuates Physical Withdrawal Signs In Opium Dependent Rats
Centers for Medicare & Medicals Services: Inpatient Rehabilitation Facilities
Addiction Science and Clinical Practice: The Neurobiology of Opioid Dependence: Implications for Treatment
Medicine Plus: Opiate and Opioid Withdrawal