Patient brokers know there’s more money in relapse than in getting people sober.
If you think patient brokering, also known as “body brokering,” is just about “professionals” getting kickbacks for referring a client to a certain rehab, you are wrong. It’s much more complicated and sinister than that. I did a deep dive and interviewed the head of a watchdog group, a rehab counselor, a rehab business development guy, and the head of an ethics association to try to get the full picture. And despite patient brokering being officially illegal in California and Florida since January, it’s still terrifyingly prevalent.
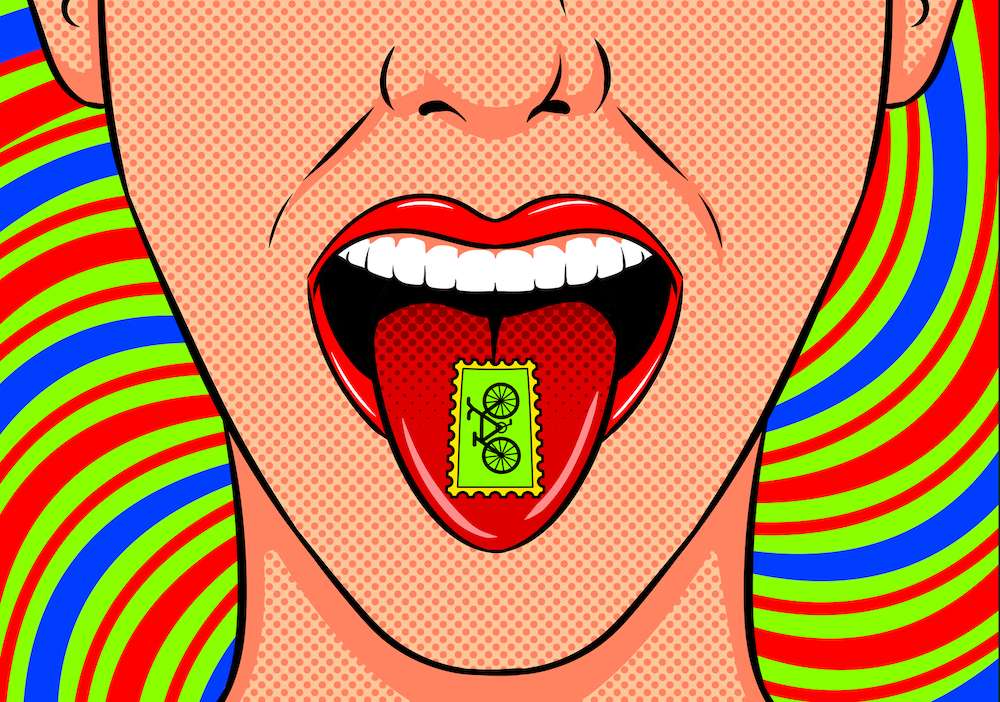
I was first prompted to write this piece after an experience with a sponsee. She was in a sober living and was offered money by another client at the house to relapse and then check into an upscale rehab. Because you must test dirty for your insurance to start over and cover treatment, she got loaded and was shipped off to a fancy Malibu rehab for a week. She was ecstatic.
Recovering Addicts Preying on Other Recovering Addicts
Of course, soon she was sent to a shitty sober living which she described as a “flop house.” Thankfully she didn’t die during the relapse, and she didn’t get her money either. The “body brokers” in this case, recovering addicts preying on other recovering addicts, ran off with the kickback money they got from the rehab as well as the money they were supposed to give my sponsee. If this sounds bad, it gets worse.
I spoke with David Skonezny, the admin for the closed Facebook group “It’s Time for Ethics in Addiction Treatment.” As Skonezny moved through the ranks of drug and alcohol counseling, eventually becoming the COO of a treatment center, “body brokering,” an open secret in the business, came to his attention. He started the group to “separate the wheat from the chaff” and to identify the people he wanted to work with to create a solution for the myriad problems plaguing the profession; however, he underestimated how pissed off and hurt people were.
“It quickly ended up being a referendum of sorts on addiction treatment as people started posting snapshots of text messages, naming names… It got really deep really fast.” As a result, one of the moderators of the group set up a site that provided a comprehensive list of agencies for the reporting of illegal and unethical activity, including credentialing and accreditation bodies, law enforcement, state agencies, and insurance investigators. People can now report the facilities as well as the brokers engaging in this illegal and unethical behavior. That site is: Ethics in Treatment (www.EthicsInTreatment.com).
“Body Brokers” Buy and Sell Patients
As Skonezny explained to me, in the referral game it’s about buying clients. Initially a treatment center might pay perhaps $10,000 for a client (that figure has dropped substantially as a result of immense competition), but it was worth it because you could bill the insurance for six figures over the course of a treatment episode. As it became harder to acquire clients this way, body brokers and rehabs started to offer other inducements such as air travel to treatment, clothes, cell phones, and cigarettes. And because people with these premium insurance policies are hard to find, brokers would find a prospect and then buy the policy for them. The rehab pays the first month’s premium, and then once the insurance is active, bingo.
Once the benefits are exhausted, however, the client gets kicked out, usually with nowhere to go and no return ticket home, and ends up homeless and desperate. But now they know the drill. They realize if they get loaded, they’re eligible for treatment again and can go back into rehab. This revolving door, “going on tour,” as Skonezny calls it, became a common strategy for both the brokers and the clients in order to maintain free housing, food, and other perks.
“This has created an artificial recovery community in Southern California, particularly in Orange County where kids are getting flown in and then kicked out. At one point it created a massive homeless population of young addicts, especially in Costa Mesa,” Skonezny told me. Some of those kids die on the streets, some go home, some keep cycling through treatment.
How did we get to this place? I asked. Well, when the Affordable Care Act went into effect, behavioral health issues, including mental health and addiction, became essential medical services.
“This created an unprecedented availability for people to get insurance coverage, and people who wouldn’t have otherwise had an opportunity to go to treatment now could,” Skonezny explained. “This should have been a good thing, except that with addicts flooding addiction centers, the owners and others began to realize that there was a lot of money to be made.”
There are two types of insurance policies: an HMO, where you need a referral from a primary doctor and must go to a place in network, and a PPO, where there’s no referral necessary and because it’s out of network, there are no contracted or set rates. Rehabs want the PPOs. They can charge whatever they want, and they do. They can bill the insurance for ridiculous amounts for daily services ($2,500 for a daily session from a PPO vs. $300 from an HMO) including huge charges for urine tests.
Alumni Get Kickbacks for Bringing in New Patients
Soon insurance companies got wise to the game and began reducing the financial reimbursement to rehabs, as well as the length and level of care they would allow. As a result, the rehabs were making less money and thus needed to up their referral game even more, so they got their alumni involved. Newly sober addicts who have been in a 12-step program have access to a network of possible patients: newcomers in meetings. These newly sober ex-clients start getting kickbacks from rehabs to bring in new clients. And then those clients do the same once they get out of treatment. Now you have a new cycle: predators creating predators.
Eventually, those people who were cycling through treatment stopped getting authorized for the higher levels of care, but they were still being okayed for intensive outpatient treatment (IOP). So IOPs began to get swarmed with clients, but these clients needed a place to live. To fill that need, sober living residences started popping up all over the place. Therein lay the beginning of kickbacks between IOPs and sober livings.
“So now we have this massive infrastructure that needs to be fed. With less clients at higher levels of care, rehabs start charging for urine testing they’re not doing and getting kickbacks from labs. Even sober livings who have no right to bill insurance for testing clients start hooking up with labs and getting kickbacks,” Skonezny said.
The people engaging in these practices are not necessarily predators by nature, Skonezny says. They are typically new to recovery and still fighting old demons and dealing with underlying trauma or other psychiatric conditions. “I think initially most people (with the exception of some of the more predatory ones) that get into this profession are well intentioned, but then greed takes over, or perhaps fear, and they begin to cut corners and engage in unhealthy, unethical, illegal behaviors.”
There’s More Money in Relapse Than Getting People Sober
Skonezny pointed out that all of it—treatment, sober livings, urine testing—has roots in legitimacy, but here’s the ugly truth: there’s more money in treatment than there is in recovery. There’s more money in relapse than in getting people sober.
Chuk Davis has 21 years in recovery and has been working in this business for over a decade. He is currently a counselor at Wavelengths Recovery and he has seen patient brokering first-hand and from the inside.
Davis explained to me the phenomenon of “client advocates.” The “advocate” calls a treatment center and says, “We have somebody who’s a really good fit for your program.” They then charge a “finder’s fee,” which was outlawed in January. “Unless you are part of the organization, you cannot be a paid recruit for the organization.” he said.
“These client advocates are really entrepreneurs: 25-year-old kids driving $50,000 cars,” Davis clarified. “Turns out they were bribing the client to come to treatment with money and a $500 gift card… The idea was they were doing some sort of vetting, but they weren’t. They were getting a fee from the center and then bribing the clients to go to treatment.”
Prior to this practice, treatment centers would contract with call centers, which would take leads and then charge the facility a certain amount of money for any lead they took. That too is now illegal.
“I’ve seen people come into treatment who say they are drug addicts but they test clean immediately. They give us some bullshit story that they already got clean but need help maintaining their sobriety. Soon enough they are paying a bunch of clients to leave and go to some other treatment center that they’re probably getting a kickback from,” Davis said. “Unfortunately, two of the people that were pulled out of treatment like this ended up getting loaded and dying.”
If Treatment Centers Don’t Pay for Patients, There’s No More Patient Brokering
Davis is hopeful that the new laws regarding patient brokering will thin the herd, and the super shady people will get pushed out. “I mean they have people talking to the local homeless and offering them $1,500 to go to some place in Long Beach for ten days. Of course those guys are going to go. In the end it’s the kids that really want help that are getting fucked.”
I next spoke with Zach Snitzer, the co-founder and director of business development at Maryland Addiction Recovery Center.
His take on patient brokering was a little different. “Patient brokering goes further than simply paying for patients. In my mind, it includes things like waiving insurance deductibles, website and call aggregates, free sober living thanks to the high payment for lab tests; not simply paying someone $1,500 to go to treatment.”
Snitzer’s answer to the brokering problem is simple: “If treatment centers don’t pay for patients, there’s no more patient brokering. If you take down the treatment centers that are doing patient brokering, then patient brokering goes away.” He’s adamant that we not only prosecute the patient brokers themselves, but the facilities engaging in it as well.
Snitzer echoed Skonezny’s observations that it’s not money-hungry crooks infiltrating the treatment industry to take advantage of people who need help, it’s people who are already here: “The patient brokers are typically people who are early in sobriety or people who were once patient brokered themselves.”
“You should be piss testing us more than you are…”
Snitzer has seen many patients who are hip to the hustle, asking what the facility is getting reimbursed, and having an insider’s knowledge of diagnostic codes. “When you have clients saying, ‘You should be piss testing us more than you are,’…well, no wonder they can’t get better.” Usually patients like that—who are already caught up in the game—don’t stay long in treatment, he said. They’re rarely initially willing to get better; for them there’s no money in getting sober.
Snitzer agreed that the ACA was a contributing factor to the problem but added that referral fees were happening way before insurance. “It’s a decades-old industry but it’s still very wild wild west. There needs to be more regulation in the industry. People seem terrified that if they don’t self-regulate, an outside agency will come in. But there are lots of industries that are regulated by outside agencies and organizations thrive in those environments.”
And state licensing is simply not thorough enough. “They don’t look at the whole scope of the organization. They don’t look at admission processing, urinalysis policies, or marketing practices… they look at hand washing stations and fire extinguishers.”
“Part of the problem is that addiction is a disease and rehab facilities are actually healthcare organizations and want to be paid and respected as such, yet they often don’t have programs that are offering evidence-based care,” Snitzer said.
“We can’t even agree as an industry about what ‘success’ looks like. Is it sobriety? That used to be what success looked like. But can that be the standard anymore? Not everyone who enters treatment is a hopeless variety alcoholic as defined by the 12 steps, and therefore maybe they don’t require lifelong sobriety to achieve a high quality of life. What about an 18-year-old kid with trauma who’s self-medicating to cope or dealing with a psychiatric issue? Do they need sobriety?”
Snitzer believes the results of effective treatment can’t be measured by the same set of criteria for everyone: “We need to figure out what a successful outcome for that person is, and it has to be defined by quality of life, and not just sobriety.”
He’s also witnessed the bribing from other facilities: vans pulling up with gift cards and other goodies, coercing patients to come to their facility in whatever way they can. “We take our clients to outside meetings and they’re approached by poachers offering to fly them out to California, claiming they have ‘music connections,’” Snitzer complained.
When I asked him how Maryland Addiction Recovery Center manages to stay ethical amidst all this, he was frank. “We don’t expand above our means. We keep things a size that’s manageable. We all started working at an ethical place [Caron]. In the mentorship we got, this kind of stuff doesn’t happen. Granted we opened in a place where there aren’t hundreds of rehabs like Florida or California. When we started, there were just a few IOPs and a few residential places but not a true extended care.”
What’s the Solution to Patient Brokering?
So now you’re well versed in the problem. What’s the solution?
Andrew Powers is in long-term recovery and has worked in the treatment field for eight years. While working for a center based in both Colorado and Maryland, he noticed several differences between the locations. Colorado treatment professionals worked in a very collaborative, transparent environment while those in the DC Metro area were more closed off.
“The cultures were drastically different,” Powers told me. He saw that people were talking shit about each other, and he thought, “Let’s raise the bar for the individuals representing treatment programs because people are receiving care at these unethical centers whether you agree with what they do or not.”
To accomplish this goal, he created the D.C.-Maryland-Virginia Professional Liaisons Association (DMV PLA), a regular forum for business development professionals, admissions representatives, marketers, and others that “focuses on the professional development of those working in these roles.”
Unlike other PLAs, which Powers found were often about referral generation and schmoozing, the DMVPLA would aim for a higher standard.
“We are working on a membership similar to NAATP [National Association of Addiction Treatment Providers], but rather than for the provider it is for the individual, which folks will be able to apply to be a part of and then held to an ethical standard of conduct,” he said. “It will be community-based at first and then we can roll it out from there… if it makes sense to do so.”
“In our field there are very limited forums for individuals working as business development, or in admissions, to receive professional development… In fact, most organizations don’t even invest in their own employees’ growth or train them on ethics at all,” Powers explained, emphasizing again that his organization is not for networking.
Like Skonezny and Snitzer, Powers acknowledges these brokers didn’t start out as predators, but that after they learn what’s going on they have an obligation to do the right thing. “There are people with good hearts and intentions working for these unethical programs, but some don’t know better,” he said. “[We’d have to tell them] ‘That thing you just saw go down, that is illegal.’ And they say, ‘Well I didn’t know it was illegal, I wasn’t trained when I got hired!’ Well now you know.”
Addiction Treatment Must Police Itself from the Inside
Powers was clear that the industry must continue to police itself from the inside. There is only so much that outside bodies can do. “People need to speak up and stop pointing fingers behind people’s backs. The term ‘marketer’ is almost synonymous with felon at this point… Let’s move toward a solution and gain the respect that our profession and roles deserve,” he urged.
The DMV PLA has received support from NAATP and others, but it’s still a work in progress. They have a lot of people reporting “well I heard…” and with that kind of vague info, their hands are tied.
Since so many people are afraid to come forward lest they lose their jobs, Powers would like to have a confidential suggestion box where people can submit anonymously and then they’ll confront that person.
Powers was humble in saying that “the DMV PLA is nothing special… just good people who came together in the community to try and make a difference in the profession, and ultimately in the lives of those seeking treatment… this can happen anywhere.”
Let’s hope it does.
View the original article at thefix.com








 I have snippets of memories of meeting
I have snippets of memories of meeting 
