The film purports to expose “how many A-list celebrities are becoming victims of Hollywood’s secret opioid epidemic and what role the studios will play in ending the crisis.”
A new documentary titled Fatal Addiction: Hollywood’s Secret Epidemic attempts to shed light on the amount of drug use among actors and other stars, particularly focusing on opioids.
Led by celebrity journalist Nancy O’Dell, the film purports to expose “how many A-list celebrities are becoming victims of Hollywood’s secret opioid epidemic and what role the studios will play in ending the crisis,” according to the synopsis.
A review by entertainment reporter Amy Zimmerman of The Daily Beast paints a picture of a sensationalizing film that puts too much blame for the opioid epidemic and other drug crises on Hollywood but that offers some important insights into the problem of Hollywood drug use.
Among the most notable insights are the stories about young actresses being pressured to take Adderall “so they can keep going and stay thin.”
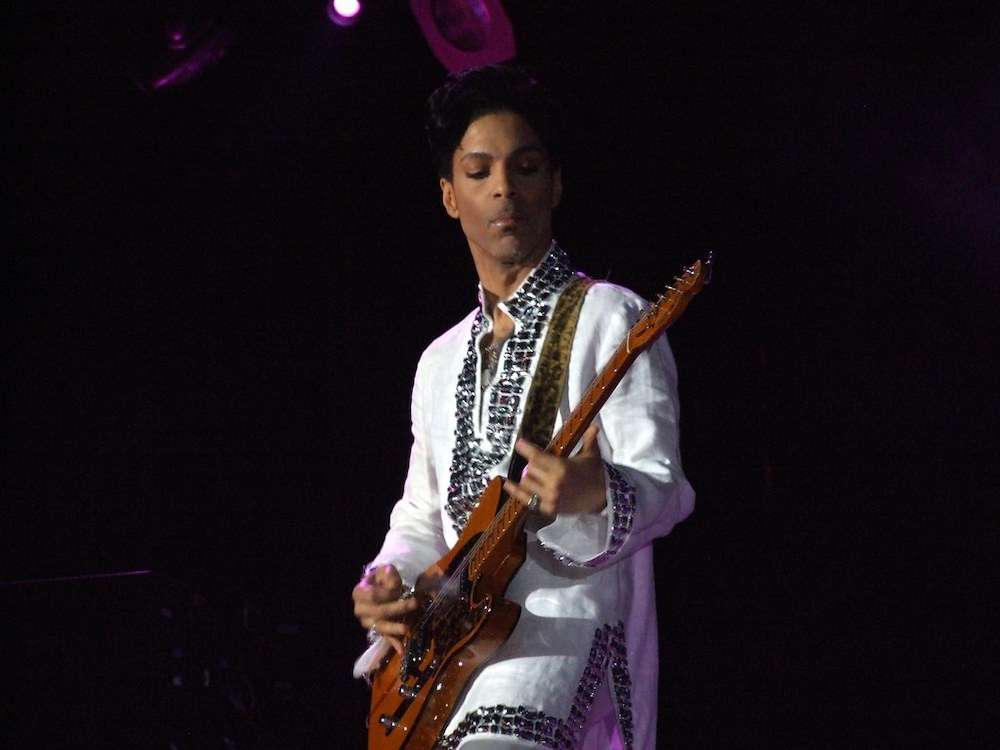
Cocktails of dangerous drugs, often involving opioids, have claimed the lives of many A-list celebrities, from Judy Garland and Marilyn Monroe to Heath Ledger and Prince. Fatal Addiction tells stories of drug use that was expected and encouraged.
“There was so much drug use on that set, it was kind of mind-numbing. And as a kid, you’re not sure how to negotiate that,” recalls Mariel Hemingway about her time filming Woody Allen’s Manhattan as a teenager.
In the case of Prince, the iconic performer was first put on opioids due to “hip problems,” and years later, by the time of his overdose, “his house was full of pills, full of opioids.” The primary drug responsible for his death was fentanyl, the synthetic opioid up to 100 times more potent than heroin.
The film does touch on the role of the pharmaceutical industry and doctors too willing to prescribe opioids in the epidemic and the deaths of many celebrities.
“Anna Nicole Smith’s doctors, as one example, are called out for ‘unbelievably bad medicine,’” Zimmerman writes, “a point that could have been made without going into extreme, gruesome detail about Smith’s state at the time of her death.”
Smith was found dead in her hotel room in 2007 and was determined to have died of “combined drug intoxication,” with all the drugs in her system being legally prescribed medications. Many celebrity overdoses have resulted from a combination of substances, particularly opioids and benzodiazepines.
“Fatal Addiction isn’t a paradigm of sensitivity and nuance, and often falters when it attempts to propose actionable solutions,” Zimmerman concludes. “But as a history of celebrity addiction and a testament to this particularly deadly era, it’s alarmingly successful.”