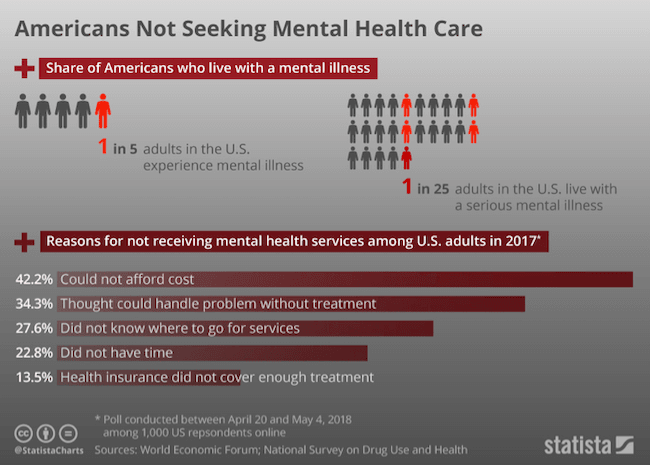
People attempting to access mental health treatment are still being denied coverage at twice the rate of those seeking physical healthcare.
A federal court has ruled that one of the largest health insurance companies in the U.S. has been discriminating against people with mental illness and addiction disorders by failing to apply coverage standards equally across physical and mental ailments. U.S. Chief Magistrate Judge Joseph C. Spero issued a “blistering” 106-page ruling stating that United Behavioral Health, a subsidiary of UnitedHealth Group, effectively discriminated against thousands of people seeking treatment for these issues from 2011 to 2017, according to The Los Angeles Times.
The Mental Health Parity and Addiction Equity Act in 2008 made it illegal for insurers to apply different criteria to patients experiencing mental health issues than those experiencing physical health issues when determining what to cover. Unfortunately, people attempting to access mental health treatment are still being denied coverage at twice the rate of those seeking physical healthcare.
According to the report by Anita Raghavan, the blame for this rests on a lack of enforcement of the 2008 law by the overstretched Employee Benefits Security Administration (EBSA).
Labor Secretary R. Alexander Acosta wrote in a 2018 report that this small division of the Department of Labor has only 400 investigators and 100 benefit advisors working to keep track of about 5 million health benefit plans across the country.
In the space of two years, the EBSA was only able to issue 136 citations to health insurance companies for violating the Mental Health Parity and Addiction Equity Act. To make matters worse, the agency can’t assess civil monetary penalties to deter future violators.
The inability to get coverage for mental health issues have left many without desperately needed treatment. This is such a common problem that the National Alliance on Mental Illness (NAMI) has a guide for what individuals can do if they’ve been denied such coverage.
This includes a list of “commonly denied types of care,” which appears to include all levels of care from diagnosis and common psychotherapy, “intermediate” care like outpatient or partial inpatient treatment, and full residential hospitalization.
Source: Statista/National Survey on Drug Use and Health
Meanwhile, reports of families struggling to get the appropriate care for mentally ill family members proliferate. In September 2018, WFYI did a story on Matthew Timion and his fight to get coverage for treatment that his adopted son desperately needed.
“He was cutting himself and he’s hearing voices and he is threatening to run away and kill me,” Timion said. “The insurance company says, ‘Well, he hasn’t done that in three or four days now, he’s good to go home.’ And the hospital said, ‘No, he has to stay.’”
The problem has become so severe that parents are increasingly resorting to giving up custody of their children because once they do, the state will be forced to pay for the necessary mental health treatment. Adoptive parents call this decision “gut-wrenching,” but without health insurance coverage for expensive treatment plans, they often have little choice.