I got a nice buzz from microdosing marijuana, but a buzz no more intense than a glass of wine sipped slowly and on a reasonably full stomach. Despite this buzz, I had no craving for more pot and I did not pick up a drink.
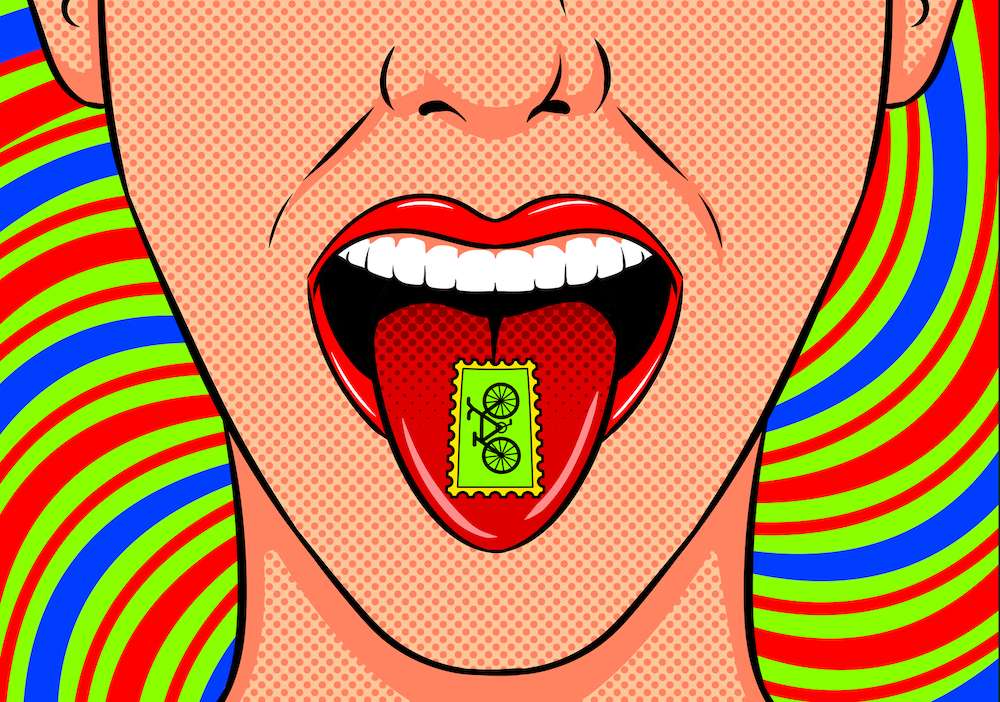
Microdosing. All the cool kids in Silicon Valley are doing it, and anyone who got sober before 2015 has been left out of the fun. At least, anyone with an all-or-nothing recovery plan, which is most people, but definitely not yours truly. Anecdotally, it looks like it’s better to have Silicon Valley hooked on low doses of LSD and psilocybin than abusing Adderall, but more empirical data on the therapeutic benefits of this trend is needed. Though I’m not going near psychedelics without a doctor’s note, I have dabbled in some microdosing on weed, and I still consider myself 100% sober.
Alcohol was my problem. It was a gnarly problem. I put the kibosh on that problem in 2009 and haven’t looked back.
Google piqued my interest in microdosing on weed by feeding me a headline that claimed one puff of it could blast away depression. I double-clicked. Since I deal with bipolar disorder and have benefited from using CBD (the non-psychoactive component in marijuana), the article seemed relevant.
According to the study, one drag of low-THC and high-CBD dose of weed can knock out depression immediately, unlike traditional antidepressants that often take a few weeks to kick in. But, there’s a catch: Continual use of THC could worsen depression, so this had to be an every-now-and-again smoke. I stored that information in my brain for future reference, noting that if I ever experienced an intense depression that didn’t abate I could give it a try since I’m fortunate enough to live in Los Angeles (pot shops on nearly every major street).
About two months after I read about the study, I got stuck in a morass of negativity and self-deprecation and self-doubt for about a week. Everything was out of alignment, and no matter how much meditation I did, I just couldn’t snap out of it. Sure, I have bipolar II, but because I take meds, 90% of the time the symptoms are manageable. Still, there are those days when stress or neurochemistry or hormones or a bad fight with a boyfriend can throw me off.
Sometimes I find relief in jogging or dancing, calling my therapist or going to a meeting, but there are times where I don’t have the energy or ability to do the very things I know will help (Depression 101). Since I’ve dealt with the condition for so long, I know when I’m dealing with a chemical imbalance and when I’m dealing with a psychological imbalance.
This time it felt like both.
I was curious to see how the weed would work, especially since I’d heard so much about the benefits of microdosing on psychedelics from friends. Because the CBD succeeded in quieting my anxiety and smoothing out my thoughts, I figured why not try something with a bit of THC.
Anyone who smokes pot can tell you that it triggers euphoria, thereby alleviating depression; you don’t need a study to tell you that. But I’ve never been a huge fan of weed, for several reasons.
For starters, my sister smoked way too much of it when she was 18, and she wound up with a permanent case of acute paranoid schizophrenia right after a three-month-long binge. Her doctor said the weed probably triggered a dormant case of the illness inherited from my schizophrenic grandfather, one that would have emerged with or without the pot, it was just a matter of time. So, that instilled in me a well-warranted dose of fear.
After staying far away from weed until my early 20s, I started smoking it every now and then, but not very often, and I certainly never purchased any or had it around. You’re probably wondering why I’d even risk smoking pot at all given my sister’s condition. Well, the doc also pointed out that she displayed many early signs of the disorder from childhood, and that my emotional and expressive–albeit mood-disordered–personality was opposite of what you’d typically see in a child predisposed for schizophrenia.
I also had passed adolescence by the time I started smoking, and the science says adolescents are the ones most at risk. Strength and frequency also play a huge role, and my sister admitted that she holed herself up in her dorm room smoking bowl after bowl after bowl all day long for months until she literally couldn’t think anymore. I had no intention of smoking more than a hit or two off a blunt.
My highs were a total mixed bag: Sometimes they relaxed me, sometimes they brought on unstoppable fits of giggles; one time I had waking dreams about dancing tortilla chips, and a few times I found myself in the midst of very uncomfortable paranoia. The one and only time I smoked way more than two hits, I wound up with full-blown psychosis that ruined an entire Halloween for multiple people. Even when smoking did bring on an enjoyable high, I still had to endure those moments of not remembering the last word I spoke, which I found, and still find, utterly horrifying. Plus my head felt like it weighed 100 pounds and my face felt like it was going to burn off.
Pot just didn’t provide an alluring buzz. I never developed a craving for or addiction to it.
If the weed I smoked had had even a small percentage of CBD, those episodes of paranoia would likely have not occurred since CBD actually curbs the anxiety-inducing effects of THC. In fact, in a bizarre twist of irony, studies have shown CBD effectively treats schizophrenia.
Sadly, whoever bred weed in the 90s and early 2000s grew strains that had little or no CBD because it decreases the psychoactive effect. (Remember chronic?) Now, CBD is making a comeback among health-conscious, microdosing millennials who are sensible enough to want a more balanced high. This is good news for a paranoid Gen Xer.
Now, you can walk into the local dispensary and see a smorgasbord of pot goodies that include CBD, from all-CBD vanilla bean cookies to 1:1 taffies to 100% CBD oil cartridges. There are salves and gums and pre-rolls and mints and a white CBD dust that looks just like cocaine, and all of them are labeled with the milligrams and the percentages of THC and CBD. This is heaven for someone like me who might want to try some pot without getting paranoid or stoned.
I have to say, I love budtenders. Mitch, who manned the shop by my house, was extremely sympathetic to my terror of coming down with pot-induced paranoia. He emphasized that dosing, strain, and CBD content made a world of difference when trying to avoid it and pointed me in the direction of 1:1 taffies. Each taffy had 5 mg of CBD and THC, which sounds low, but it’s no microdose for someone like me. According to Mitch, 5 mg of CBD and THC can lead to a strong high for someone with zero pot tolerance, and I wasn’t looking to get stoned — I just wanted that mild euphoria, for the bell jar to lift.
I ended up buying the taffies and slicing them into thirds, which Mitch suggested. In the end, I was ingesting about 1.5 mg of THC and 1.5 mg of CBD, which a lot of doctors would consider an ineffective dose, but not for me! My brain is super sensitive. After two hours, I ended up feeling a very small effect, but of course it grew.
Ultimately, the high — if you’d call it that — was a powerful feeling of ease and positivity. My thoughts quieted, and yes, a mild euphoria fell over me. It was, without a doubt, a nice buzz, but a buzz no more intense than a glass of wine sipped slowly and on a reasonably full stomach. Despite this buzz, I had no craving for more pot. I was so pleased to not be paranoid or forgetting my thoughts as they spilled out of my head, the last thing I wanted was more. More might have induced those adverse effects. (Oh, the benefits of legalization!)
I am not ashamed of that pot buzz nor do I think it nulls my sobriety in any way. My sobriety is just that — my sobriety, and it’s not some stringent moral code that demands I never feel any psychoactive pleasure whatsoever just because I used to drink myself into rages, sobs, and blackouts. If the pot buzz was harmless and actually beneficial for my mental health, why not embrace it? One of the main reasons I got off the booze is because how seriously destabilizing it is for my mood given my bipolar diagnosis. When I drank too much, it sent me crashing down into suicidal depressions.
Normal drinkers get a slight buzz — if not a big buzz — from their drinks, and they’ll admit it. It’s a social lubricant and a relaxant that well-adjusted and healthy folks leverage all the time to take the edge off and have fun. When they manage to leverage these positive aspects of alcohol without destroying their lives, we tip our hats to them.
Being out of AA for nearly three years no doubt helped me take the microdosing plunge with zero guilt.
Now, if I wanted to gorge myself on those taffies after this experience, that would be problematic, at least for me. Someone else might not care if they engage that behavior, but I’m not in the mood to pick up any new addictions.
I’m still very wary of using weed on the regular given my familial history of schizophrenia, though at this age my chances of developing the illness are low. Some studies have shown that heavy and regular use can fry your short-term memory, and I’m not down for that either: I need all the synapses I can get as I push 40. So, I don’t plan on using it very often.
After having the weed, the positive mood lasted for a few days without ingesting any more taffies. I basically just returned to baseline. I didn’t eat any for weeks after that episode. Since then, I’ve probably had two or three, each time cutting them in thirds or halves. After a while, the package just sat there in the fridge, and eventually I ended up tossing them when I moved out of the apartment.
So, now I have no taffies, and I could frankly care less. If I feel like one might help me in the future, I’ll take it. If I go out to the desert, maybe I’ll take some for recreational use. Either way, I know my limitations, and I know I don’t want to do it often. Because I don’t experience a craving, I doubt this will be a problem. I experienced a craving for alcohol from Day One. From the very beginning, I needed more.
“Marijuana maintenance,” or smoking pot in recovery, is generally frowned upon by your standard AA member. Historically referred to (incorrectly) as “the gateway drug,” 12-step philosophy looks at it in the same way, cautioning that if you start smoking it in recovery it will open up the floodgates toward drinking again.
The problem with this thinking is that it doesn’t take into account the vast differences that exist between all of us, be they physiological or psychological, or, hell, even spiritual. After reading much about recovery, from Lance Dodes to Marc Lewis to Gabrielle Glaser to Bill Wilson and all the stories in the rest of the Big Book, I feel that it’s unconscionable to argue that we are not unique, as so many people do in 12-step programs. We are highly unique, and observing this and tailoring treatment plans for each individual will increase success at recovery. One-size-fits-all recovery modalities are, according to my research, quite dangerous.
Imagine if a woman with breast cancer walked into a doctor’s office and the doctor said, “Well, there’s no reason to take any additional imaging because all breast cancer patients are the same. You’re not unique. Mastectomy it is!”
Even in the dark ages medicine was probably more sophisticated than this. So why are we in the dark ages when it comes to addiction treatment? If our bodies are this unique, then so are our minds. The field of psychiatry also takes our differences into account, with medication and other treatment prescribed according to individual circumstances.
I am not encouraging anyone to microdose, but I am trying to encourage the sober community to keep an open mind about new psychotherapeutic treatments and to accept the fact that some people can stay away from their drug of choice while indulging in a substance that wasn’t and isn’t problematic. Studies have shown that marijuana can benefit our mental health; let’s continue to study this promising medicine instead of closing ourselves off to it out of fear.
Microdosing on anything while in recovery is a very nuanced topic, and drawing blanket conclusions won’t do anyone a bit of good. But in order to make room for these conversations, we have to be open and accepting. We have to be willing to say, “Okay, she can take a little THC every now and then and enjoy it. I know it’s not a good idea for me since I smoked too much pot in the past, so I won’t do it.” We all need to be in touch with our own limits and accept them while not imposing them on others; otherwise, we resort to reductive fear-mongering that has no basis in reality.
View the original article at thefix.com